
What is psoriasis?
Psoriasis is a chronic condition that causes red, itchy scaly patches on the skin. Psoriasis may also affect other parts of the body or organs. There is no cure for psoriasis, but it can be managed with the right treatment.
The severity of psoriasis varies widely between people. For most people, it will be mild and can be treated with topical treatments (treatments such as creams that go on the skin). The appearance and severity of a person’s symptoms will vary over time, and so will their treatment needs.
One in three people with psoriasis may develop psoriatic arthritis (PsA), a related disease which causes inflammation of the joints. People with psoriasis may also be at higher risk of developing other health conditions such as heart disease, diabetes and depression.
Signs and symptoms
Psoriasis causes skin cells to grow rapidly and build up on the surface of the skin. This gives the appearance of red, thick, scaly, dry, patches (plaques) that can be itchy and painful. The skin signs of psoriasis can look similar to other skin conditions, so it is important you receive the correct diagnosis.
Common signs and symptoms of psoriasis include:
- raised, red, inflamed lesions covered in silvery scales (referred to as plaques)
- small, red, individual spots, which can be flat or raised
- dry skin that may crack and bleed
- itching, burning, or soreness of the skin
- thickened, pitted nails or separation of the nail from the nail bed
There are different types of psoriasis that may cause different symptoms. The most common types of psoriasis, include:
Plaque psoriasis: This is the most common type. The affected areas of the skin appear as thick, raised scaly patches.
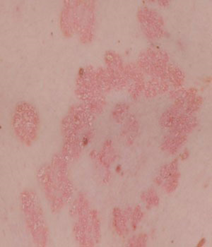
Image appears with permission from the Skin Health Institute
Guttate psoriasis: More commonly seen in children, teenagers and young adults, often following a throat infection known as Streptococci. It causes widespread small red spots, commonly on the torso, arms, and thighs.

Image appears with permission from Getpsorted
Pustular psoriasis: This type of psoriasis is uncommon and mostly occurs in adults, particularly smokers. Pustular psoriasis causes small 'blisters', surrounded by red skin.

Image appears with permission from the Skin Health Institute
Palmoplantar psoriasis: This type affects the soles of the feet and palms of the hands. Thick, red, scaly patches of skin appear and develop painful cracked skin.
Inverse psoriasis: Typically appears as red, smooth patches in the folds of the skin (e.g. armpits, groin, under the breasts and between the buttocks).
Erythrodermic: This is a severe form of psoriasis that affects most of the skin on the body with widespread redness. It is a rare form of psoriasis and is considered a medical emergency that requires prompt treatment.
Changes to the fingernails or toenails
Another sign of PsA may be changes to the look and structure of the nails on the fingers or toes.
Pitting of the nails (small shallow dents in the nails) is the most common symptom in people with PsA. It is caused by inflammation of the tissue that causes nail growth.
Another common change to the nails in people with PsA is when the nail lifts away from the nail bed underneath (known as onycholysis). This can increase the risk of infection, so it is important to practice good hand hygiene.
Image appears with permission from VisualDx/Skinsight
What causes psoriasis?
The exact cause of psoriasis is unknown. One in three people with psoriasis will have family members with the condition. However, this does not necessarily mean you will develop psoriasis yourself. Genetic factors may increase your risk, but environmental factors may also play a role.
An overactive immune system is known to play an important role in driving the disease. Many treatments work by suppressing the immune system, to help reduce inflammation.
Psoriasis is not contagious, meaning it cannot be passed from one person to another. It is not caused by dirty skin or poor hygiene.
While we do not know the cause of psoriasis, we do know there are several “triggers” that may make psoriasis worse:
- Stress can cause psoriasis to flare up for the first time or can worsen existing psoriasis.
- Damage to the skin (such as sunburn, cuts, and scratches) can cause psoriasis to appear.
- Some medications can worsen psoriasis including some anti-inflammatory drugs and certain heart and blood pressure medications (‘beta-blockers’).
- Bacterial infections and certain viruses can trigger psoriasis for the first time or worsen existing disease.
- Changes in hormones, such as in pregnancy, can cause changes in psoriasis severity.
- Smoking increases the risk of developing psoriasis and the severity of the disease.
How is it diagnosed?
Only a healthcare professional can diagnose psoriasis. In most people, psoriasis can be diagnosed based on how the rash looks.
Tests may be needed to rule out other conditions (e.g., skin scrapings for fungal infections), or before starting treatment (e.g., blood tests).
Some question-based tests may also be used to assess the extent and severity of your psoriasis and how it affects you. For more information, please visit www.getpsorted.com.au.
What will happen to me?
Psoriasis can affect people in different ways. Some people will find they only have mild psoriasis that can be treated topically (creams, lotions, ointments etc.). Others may have severe psoriasis that affects many parts of their body, (e.g., scalp, torso, and nails) and require stronger medications or ultraviolet light treatment (phototherapy).
The good news is that psoriasis can be treated, and your symptoms can improve.
It is important you speak to your doctor if you experience any other symptoms, such as joint pain, which may be a sign of PsA.
Is there a cure for psoriasis?
There is no cure for psoriasis, which means that there are no treatments that will make it go away forever. However, there are many treatments that are very effective, and most people can achieve ‘normal-looking’ skin. Psoriasis does not scar but can leave pigmentation (darker patches of skin).
Treatments
There are a variety of treatments for psoriasis which come in different forms. A GP or dermatologist (specialist skin doctor) will recommend the treatment that is best for you.
Treatment of psoriasis starts with avoiding the triggers (mentioned above) that can make it worse.
Read our Treatments for psoriasis article for more information on the types of psoriasis treatments.
What can I do?
There are several things you can do to help treat and manage your psoriasis, you can:
- Speak to your doctor to get the right diagnosis and treatment to help manage your condition. Treating your psoriasis effectively and maintaining your general health can reduce the risk of developing other health conditions associated with psoriasis.
- Maintain a healthy weight by exercising regularly, eating a healthy diet and moderating your alcohol intake.
- If you smoke, try to quit as smoking may worsen your psoriasis. Speak with your doctor about ways to help you stop.
- Acknowledge your feelings and seek support. Some people with psoriasis may feel depressed, anxious, and embarrassed. Psoriasis might affect the type of clothes you can wear and your ability to do daily activities. This can all add to feelings of low mood, which can trigger a psoriasis ‘flare’. Be aware of these feelings and get help if they start affecting your daily life.










